The HelpMeSee Simulation-based Training model is helping revolutionize ophthalmology care.
Approximately 100 million individuals worldwide are living with avoidable blindness or significant visual impairment due to cataract. (1) Of them, about 90% live in under-resourced countries, where significant geographic and economic hurdles must be overcome to receive adequate eye care. (2,3)
The consequences of blindness, especially in low-resource countries, are dire. Adults with blindness have a one-third shorter life expectancy compared to those with healthy vision, and blind children are at significant risk of mortality in the first year of losing their vision. (4) Yet the impact of cataract blindness burdens more than the sightless individuals themselves, who are pulled from the workforce or school depending on their age. Young children often drop out of school to care for a blind family member or neighbor, magnifying the suffering of sightlessness and reducing productivity and the ability to contribute financially.
Much of the negative impact of cataract-related blindness and significant visual impairment can be mitigated with better access to quality eye care. With a sizeable shortage of cataract surgeons relative to patient demand and substantial geographic disparities, (5) safe, effective, and reproducible surgical training modules are more important than ever before to bridge the gap between the growing cataract blindness population and the increasing surgeon shortage.
Traditionally, cataract surgery training follows an apprenticeship model, with trainee surgeons learning in a wet lab setting, observing experienced surgeons, and progressing to performing parts and eventually entire surgeries under supervision.
Although this approach provides crucial hands-on experience, it also has several limitations, including dependency on mentor and technology availability, limited exposure to complex cases and a variety of surgical techniques, potential increased risk to patients during the learning curve with new procedures and techniques, subjectivity in the assessment of trainee proficiencies, and lack of objective feedback mechanisms.
Inexperienced and experienced surgeons alike can make mistakes, even during routine procedures. (6) This highlights the need for innovative training models that address the inherent limitations of traditional cataract surgical training. Today, there are several training methods that allow trainees to practice their surgical skills in a controlled and effective learning environment. Among them is the HelpMeSee Simulation-based Training program.
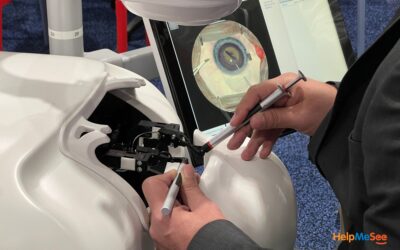
HelpMeSee is a leader in ophthalmology technology, reshaping the landscape of trainee education. The HelpMeSee Eye Surgery Simulator replicates the intricacies of the ocular anatomy and offers trainees a safe and controlled environment for surgical skills acquisition and proficiency assessments without risking patient safety. Trainees use instructor-led, standardized methodology on a visual and tactile virtual reality simulator to minimize the learning curve, decrease intraoperative complications, and improve patient safety. (6)
The advantages of simulation-based training are multifaceted. It provides trainees with unlimited opportunities to repeat procedures, perfect their technique, and enhance their competence and confidence. Simulation-based training also allows standardization in curriculum delivery to ensure consistency in skills acquisition across diverse learning environments and in performance metrics to facilitate objective feedback and competency-based progression.
In one study, use of the HelpMeSee Eye Surgery Simulator reduced surgical errors by about 50%, demonstrating its efficacy in preparing cataract specialists for real-life scenarios. (7)

According to Lansingh and colleagues, a surgical simulator “provides an environment where a trainee can not only learn the right technique to perform a particular surgical step but also intentionally make mistakes over and over again. This would teach them how to avoid surgical complications as well as how to manage them, depending on the fidelity and complexity of the simulator. Even very rare complications, which a surgeon may encounter perhaps once during a working lifetime, can be faced and managed appropriately.” (8)
Also important, the impact of simulation-based training with the HelpMeSee Eye Surgery Simulator extends beyond individual trainees and institutions. It democratizes access to high-quality surgical education, particularly in underserved regions, thereby contributing to a broader global eye care agenda and addressing critical shortage of trained cataract surgeons.
Local eye care providers become empowered with the specialized skills learned through simulation-based training, laying the foundation for long-term systemic change and sustainability in global eye care.
Learn More About Training in Your Region
Instructor-led Simulation-based Training Courses
Learn More About Training in Your Region
Instructor-led Simulation-based Training Courses
Learn More About Training in Your Region
Instructor-led Simulation-based Training Courses
HELPMESEE SPONSOR’S






- GBD 2019 Blindness and Vision Impairment Collaborators; Vision Loss Expert Group of the Global Burden of Disease Study. Causes of blindness and vision impairment in 2020 and trends over 30 years, and prevalence of avoidable blindness in relation to VISION 2020: the Right to Sight: an analysis for the Global Burden of Disease Study. Lancet Glob Health. 2021;9(2):e144-e160.
- Orbis International. Global blindness was slowing prior to pandemic study reveals. Accessed February 22, 2024. https://www.orbis.org/en/news/2021/new-global-blindness-data
- International Agency for the Prevention of Blindness. 1.1 billion people live with vision loss. Accessed February 22, 2024. https://www.iapb.org/learn/vision-atlas/
- Etya’alé D. Eliminating onchoceriasis as a public health problem: the beginning of the eye. Br J Ophthalmol. 2002;86(8):844-846.
- Berkowitz ST, Finn AP, Parikh R, Kuriyan AE, Patel S. Ophthalmology workforce projections in the United States, 2020 to 2035. Ophthalmology. 2024;131(2):133-139.
- Lansingh VC, Gonzalez PD, Díaz Flores T, Lopez Star EM, Martinez JM. How many cataract surgeries does it take to be a good surgeon? Revista Mexicana de Ophthalmologia (Eng). 2023:10.5005/rmo-11013-0026.
- Nair AG, Ahiwalay C, Bacchav AE, Sheth T, Lansingh VC. Assessment of a high-fidelity, virtual reality-based, manual small-incision cataract surgery simulator: A face and content validity study. Indian J Ophthalmol. 2022;70(11):4010-4015.
- Lansingh VC, Ravindran RD, Garg P, et al. Embracing technology in cataract surgical training – the way forward. Indian J Ophthalmol. 2022;70(11):4079-4081.
RECENT NEWS
Pars Plana Vitrectomy: Why It’s Important To Master and How To Do So
Pars plana vitrectomy (PPV) is a sophisticated surgical technique used for the management of various vitreoretinal disorders by providing access to the...
Women in Ophthalmology: Overcoming Obstacles and Embracing Technology
Significant strides have been made to increase the representation of women in medicine. In ophthalmology, specifically, the journey toward gender equity...
Objective Feedback Maximizes Learning in VR Eye Surgery Training
Feedback is a crucial component of cataract surgery training programs. It enables trainees to learn from experienced surgeons how to refine their skills...