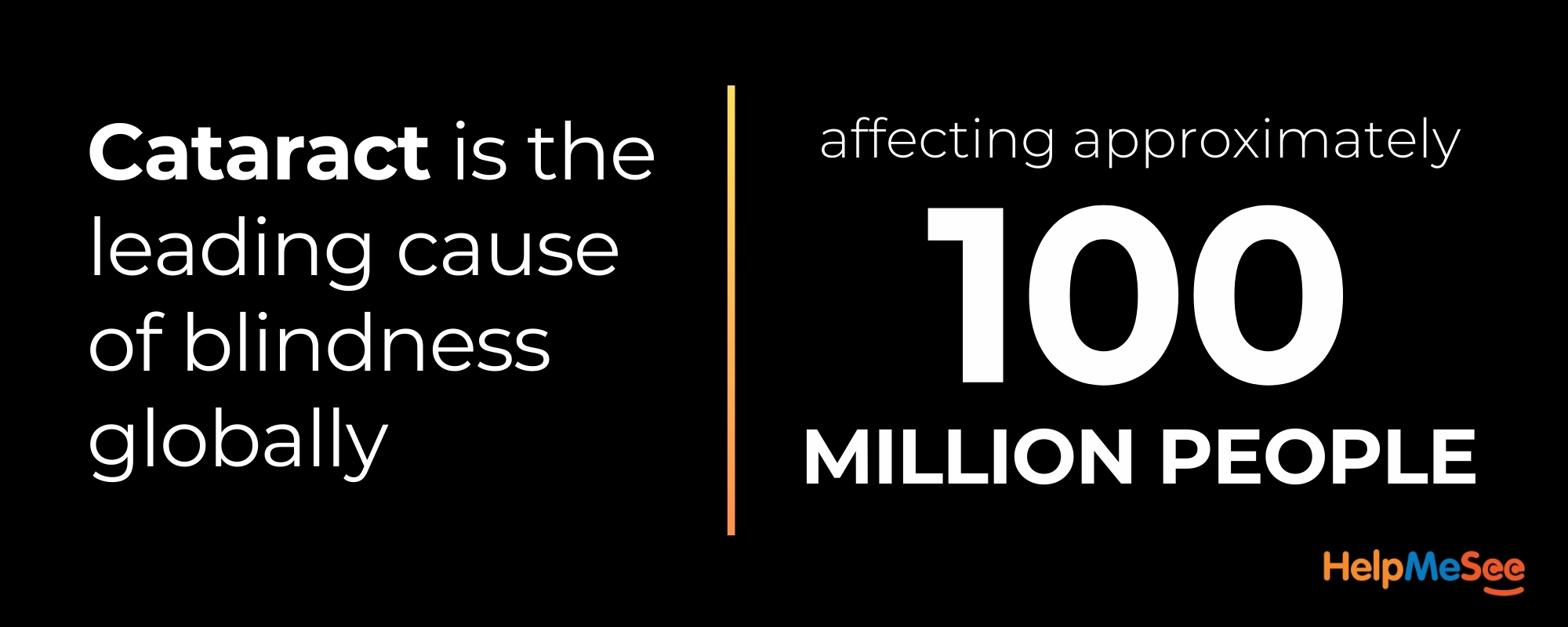
Phacoemulsification is the predominant cataract surgery technique in the United States. In other parts of the world, especially in low-resource settings, Manual Small Incision Cataract Surgery (MSICS) is a low-cost alternative. Although the value of learning MSICS during residency training in the United States might not seem immediately apparent, studies have shown that mastering MSICS may help reduce the learning curve for phacoemulsification. (1) It may also prove useful in complex cataract surgery cases in which a surgeon must pivot from phacoemulsification due to extreme density of a cataract or corneal opacity as well as other conditions such as pseudoexfoliation and disorders of the corneal endothelium. (2-6)
CASE STUDY: COLUMBIA UNIVERSITY OPHTHALMOLOGY RESIDENCY PROGRAM
Royce W. Chen, MD, Ophthalmology Residency Director and Vice Chair of Education at Columbia University, has seen the benefits of simulation-based MSICS training firsthand. “By the time residents come back into the operating room—even though they were doing MSICS simulation training and not phacoemulsification—the mere act of spending time under a microscope with an instructor who is pointing out tips and what they could do differently in terms of hand position translated into a more advanced understanding of phacoemulsification,” he said, adding that residents tend to adopt a more accelerated pace of development compared to those who don’t undergo simulation training.
Columbia University partners with HelpMeSee to provide simulation-based surgical training to its residents. Dr. Chen has worked closely with HelpMeSee, acknowledging that the relationship deepened during the COVID-19 pandemic when robust and flexible surgical training was paramount to keep residents engaged and active during the lockdown and its aftermath. “During pandemic time, there was a 3-month hiatus in elective surgery. That was when we started working with the HelpMeSee simulator more frequently,” he said. “We found it was a wonderful simulation tool for surgical training because of its haptic feedback and its high-fidelity representation of the surgical experience that felt very realistic.”
Since 2020, HelpMeSee has refined and built out its curriculum to include other surgeries including phacoemulsification. Now, Dr. Chen says, his residents focus on the HelpMeSee Phacoemulsification Module. “The modules are really robust and do a very good job of preparing trainees. We are very happy to have that as part of our training program,” he said.

The concentrated 40-hour training block with HelpMeSee allows residents to develop fine motor skills, hand positioning, and spatial awareness—all under the close supervision of a dedicated instructor. These lessons, which at Columbia University are typically offered in postgraduate year 3, right before their final year of surgical training, prove transferrable when residents return to the operating room for the majority of their surgical caseload, accelerating their learning curve for all types of cataract surgery, Dr. Chen emphasized. “When they’re ready to really ramp up surgical volume, they can do so … in a safer fashion.”
A key advantage of the HelpMeSee Simulation-based Training Program is the structured instructor-led learning model, which is “very different from any other training model I’ve seen previously,” Dr. Chen said. “It is not a passive learning experience where residents are expected to work on a simulator by themselves—which is what I did as a resident—and I really came to appreciate that … the resident is with a dedicated instructor going through all the steps with required pre-reading. They have to understand what they’re going to do, and then they actually go through the simulation. They can’t advance to the next step until they pass the current step.”
Dr. Chen has noticed greater technical proficiency and increased confidence in his resident’s surgical abilities now that they use HelpMeSee simulation training. “It’s the best high-fidelity simulator that exists. I think it is the greatest value for our residents. … We have uniformly positive feedback from our residents,” he said. The repetitive, controlled practice in a high-fidelity simulation environment creates muscle memory and surgical intuition that translates into improved performance across the board. Moreover, MSICS is a vital procedure globally, particularly in low-resource settings, and US surgeons with MSICS skills are better equipped to contribute to international humanitarian efforts—a core mission of HelpMeSee.

THE FUTURE OF RESIDENT TRAINING
The partnership between Columbia University’s Ophthalmology Residency Training Program and HelpMeSee highlights the importance of simulation-based education in ophthalmic training. MSICS training, while not the primary focus in the United States, may be included as an essential part of developing well-rounded, skilled cataract surgeons.
The HelpMeSee high-fidelity simulator and instructor-led training ensures that residents not only learn the technical aspects of MSICS and Phacoemulsification (among other surgical modules) but also gain the confidence and competence necessary for success in the operating room. Through partnerships like these, the ophthalmology community is better equipped to teach the next generation of ophthalmologists.
Learn More About Training in Your Region
Instructor-led Simulation-based Training Courses
Learn More About Training in Your Region
Instructor-led Simulation-based Training Courses
Learn More About Training in Your Region
Instructor-led Simulation-based Training Courses
HELPMESEE SPONSOR’S







- Lynds R, Hansen B, Blomquist PH, Mootha VV. Supervised resident manual small-incision cataract surgery outcomes at large urban United States residency training program. J Cataract Refract Surg. 2018;44:34-38.
- Bourne RRA, Minassian DC, Dart JK, Rosen P, Kaushal S, Wingate N. Effect of cataract surgery on the corneal endothelium: Modern phacoemulsification compared with extracapsular cataract surgery. Ophthalmology. 2004;111:679-685.
- Bhargava R, Kumar P, Sharma SK, Arora Y. Phacoemulsification versus manual small incision cataract surgery in patients with fuchs heterochromic iridocyclitis. Asia Pac J Ophthalmol (Phila) 2016;5:330-334.
- Venkatesh R, Tan CS, Sengupta S, Ravindran RD, Krishnan KT, Chang DF. Phacoemulsification versus manual small-incision cataract surgery for white cataract. J Cataract Refract Surg. 2010;36:1849-1854.
- Malik, Krishan Pal Singh; Goel, Ruchi1. Why learn manual small-incision cataract surgery?. Indian Journal of Ophthalmology 70(11):p 3753-3754, November 2022. | DOI: 10.4103/ijo.IJO_1944_22
- Editor, By Liz Hunter, Senior. “The Right Time for MSICS and MiLoop.” Www.reviewofophthalmology.com, www.reviewofophthalmology.com/article/the-right-time-for-msics-and-miloop.
RECENT NEWS
Increasing Cataract Surgery Access: Mission Critical
Individuals with cataract-related vision loss or blindness may mistakenly believe that their condition is permanent. The truth is, however, cataract...
The Power of Cataract Simulation-Based Surgery Training
Virtual reality–based surgical simulation-based training is a win-win for residents and residency program directors. It can be used to teach vital surgical skills…
Embarking on a Life-Changing Journey
Cataract surgical training is evolving. While most residency programs use an apprenticeship model, allowing trainee surgeons to progress…




